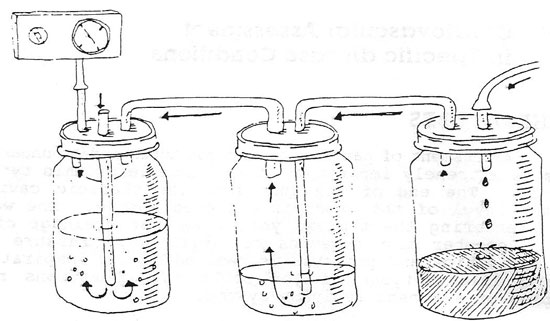
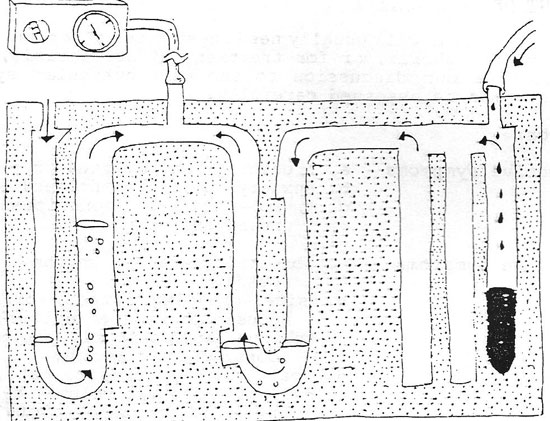
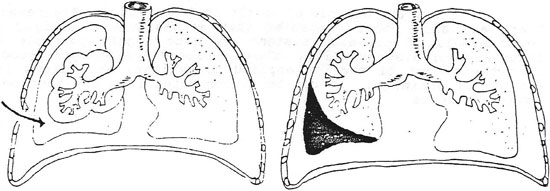
Part V: Cardiovascular Assessment in Specific Disease ConditionsChest TubesAssessment of patients with chest tubes and/or underwater drainage systems is extremely important. The principle of this type of drainage is simple. The end of the tube from the thoracic cavity is placed below the level of the water in the closed bottle. The water prevents air from entering the thorax, yet allows for drainage of the pleural space. Remember the dynamics of breathing; pressure is increased during expiration and pressure is reduced during inspiration. See the following illustrations if you still have questions regarding the principles of a closed drainage system. Assessment of the Patient A patient will usually need chest tubes after any type of surgery that enters the thorax, or for treatment of atelectasis, etc. We will try to confine our discussion to the cardiovascular system, but the lungs must also be assessed carefully. Assess for:
Study the example of bottle drainage and the Pleurevac system. There are also other companies that manufacture a similar product. Newer models of drainage systems are made highly portable and with fewer ways of disconnecting. These enclosed systems give good control over the amount of suction applied to patient, and allows for large amounts of drainage. It can be disconnected from the suction with no adverse effects.
Peripheral Vascular Disease When we discuss peripheral vascular diseases, we will limit the topics to the most common ones. Many of the diseases of the vessels in the extremities will not be observed by most nurses, as these patients are usually treated in the doctor’s office and rarely reach the hospital. Peripheral vascular problems can be divided into two main sections dealing with arterial problems and then venous problems. As you know, peripheral vascular disease is defined clinically as ischemia to a part due to decreased circulation. In this section we will concentrate on assessment concerning peripheral vascular disorders dealing with both the arterial system and the venous system. Below are some criteria to use for assessing these conditions. Keep in mind that these criteria below are primarily for the acute disease conditions. Chronic occlusive disorders will tend to cause chronic problems with pain and sensory and/or motor systems. Chronic disorders are usually asymptomatic at rest, and then symptoms appear or get worse on exertion. Arterial Vessel Assessment: Begin by performing the routine assessment that you would for any patient. Begin with vital signs, routine pulse determinations, including pedal pulses, and then proceed to the more specific assessment below (Sexton 85, Taggert 85)
Venous Disease Assessment Peripheral venous problems usually develop from increased venous pressure. These conditions may include: valve damage from inflammation or stretching, dilation from defective vein walls, thrombus formation secondary to endothelial lining damage, venous stasis, or hypercoagulability. The symptoms of peripheral venous vascular disease will usually also correspond to the extent of the damage of the vessels. Also remember that today there are many sophisticated ways of diagnosing peripheral vascular disease. However, they still do not replace a through hands on assessment from the nurse. Acute disease assessment: Acute peripheral venous disease is usually associated with conditions such as immobility, dehydration, blood dyscrasias, and malignancies. Acute phlebitis and acute thrombophlebitis are the most common problems. One of the major indicators of peripheral venous conditions is edema. Increased hydrostatic pressure within a vein can cause a fluid shift into the interstitial space, edema is the result. Assessment should include recording any edema and the amount present. First, you inspect both legs for symmetry in color, temperature, and size. In some cases, you may need to measure the exact diameter of the leg at various points in order to detect if the problem might be getting worse. Measure the leg at several different points with the same tape measure and at the same points every day. You may have to mark the exact locations on the leg to be sure that you are measuring the same place every day. Continue your assessment of the patient by gently palpating the legs for nodules, lumps, or inflamed veins. Assess for Homan’s sign as well as for general feeling of malaise, fever, or fatigue which are often present with inflamed veins. Chronic disease assessment: The symptoms seen with chronic peripheral venous disease are similar to those of the acute type. Those with chronic disorders however, will tend to have other medical problems and tend to have both legs involved. Some symptoms might be: chronic pain and edema, cramping, fatigue in legs after standing or sitting for short periods, there is often more discomfort at the end of the day. Also assess for feelings of burning and itching of the legs that usually is due to a buildup of catabolic wastes. This might also lead to an exzematoid dermatitis. Their legs feel heavy and tight. Assess also for skin ulcers, pigmentation, and trophic changes. In Summary: It is sometimes very difficult to differentiate between peripheral arterial and venous conditions. When there are many systemic and chronic medical problems present, along with edema and/or fatigue in the extremity, chances are the problem is venous. When the symptoms include numbness, tingling and/or sensory and/or motor changes, the indications might indicate an arterial problem. Whichever is the case; the nurse must still assess the patient very carefully and keep in mind the immediate nursing measures that should be taken. Next: Part V: Cardiovascular Assessment in Specific Disease Conditions, Con't. |